
What is the FODMAP Diet?
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|

|
|
|
|
|
|
|
|
|
|
|
|
|
|
|

AUG 06, 2024
How Healthy Are Gummy Vitamins? These days taking gummy vitamins can be sweeter than ever. But is it good for you? Growing number of companies are selling gummy vitamins ranging from multivitamins to collagen. They look and taste a lot like candy. Come in all different colors, size and playful shapes. But the sad reality is they are ineffective, possibly harmful, and a complete waste of money. Too Much Sugar There are many doctors that are saying buyer beware of gummy vitamins. Gummy vitamins contains sugar. Gummy vitamins can carry 2 to 8 grams of sugar which means 90% sugar and 10% vitamins. That is like getting 90% ice and 10% drink. If you think sugar free gummies are better, there are some concerns as well. Sugar free gummies contain sugar alcohol which can cause unpleasant GI affects like bloating, gas, diarrhea, and abominable pain. Consumer labs (consumerlabs.com) is consumer advocacy organization that has done some extensive research about the problems with gummy vitamins has stated that there is more sugar (nearly up to 90% sugar than vitamins). In addition, sugar alcohol taking daily may lead to diarrhea, stomachaches and bloating. Low Quality means No Benefits Another issue with gummy vitamins is quality. Gummy vitamins lose potency faster when it’s in gummy form (Consumerlabs.com). In other words, they may not even work. The label on gummy vitamins are not accurate because the it loses potency over time. If you are taking collagen gummies you may be taking less than .5 gram of collagen which like taking no collagen. Some manufactures overcompensate by adding more potency which can be harmful as well. For example, fat-soluble vitamin gummies like A, D, E, and K can build toxic levels in the body if take in excess. (WebMD). Artificial Ingredients Gummy Vitamins often contains artificial food dyes and fillers to give them appealing textures (WEBMD). It should be noted that vegetarian gummies vitamins are made with pectin which is derived from citrus fruit peels and apples. The problem with pectin is it must be combined with other substance like sugar and acids (methoxyl). Solutions Don’t take gummy vitamins. Gummy vitamins have many downsides, compared with traditional supplements. The dosage of gummy vitamins can be unreliable. Also, chances are that by the time you eat your gummy, its vitamin content will have degraded. The better option is to take traditional pills, powders, capsules and tablets. Don’t take gummy vitamins, collagen, creatine etc Take capsules Take powders Avoid Pectin, sugar alcohol and sugar based gummies
READ MORE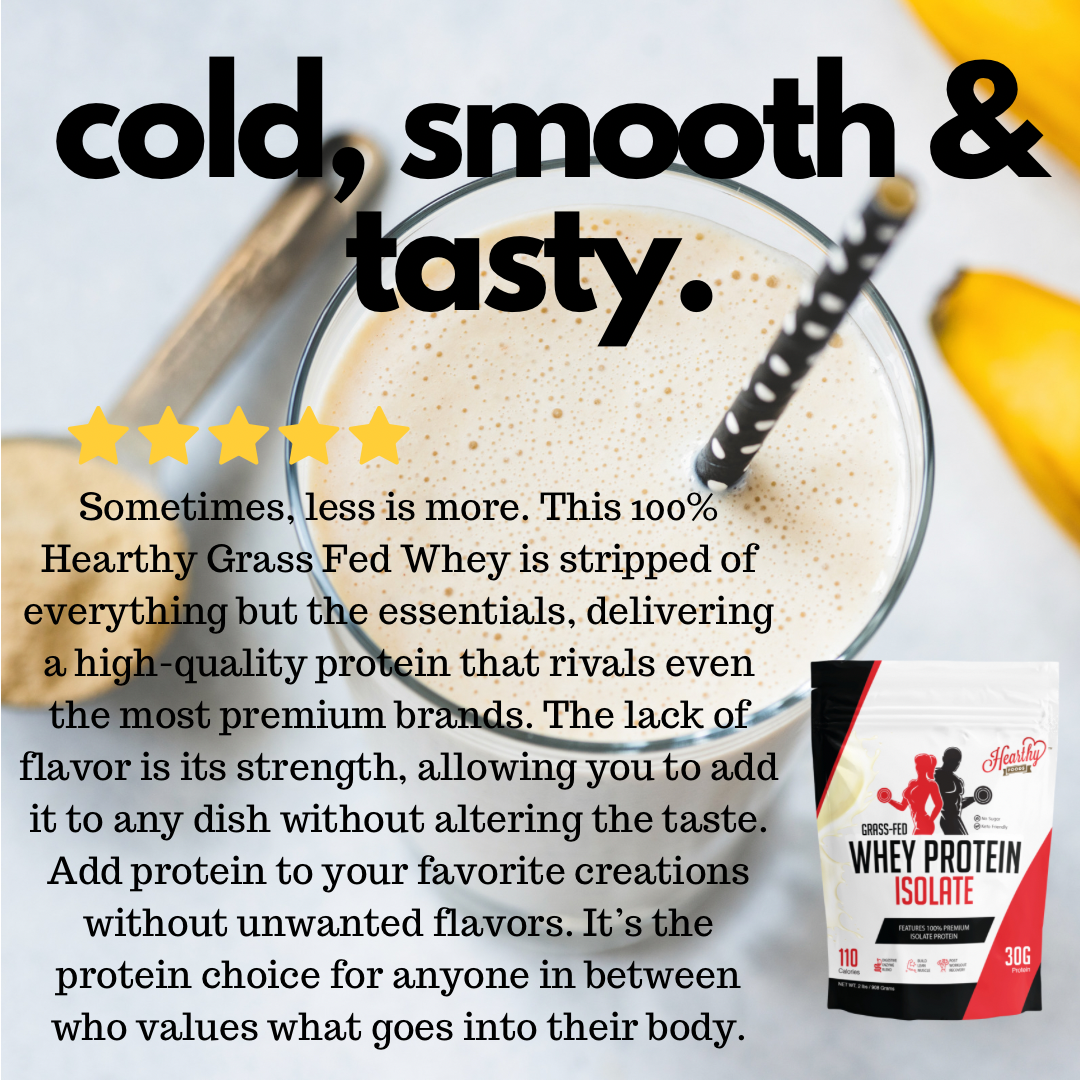
AUG 14, 2024
Hearthy Grass Fed Whey is a high-quality protein supplement with several key features. Here’s a detailed breakdown:Key Features: 1. Grass-Fed Source: The whey protein is derived from cows that are grass-fed, meaning they are raised on a natural diet of grass rather than grains. This is often associated with higher levels of omega-3 fatty acids and CLA (conjugated linoleic acid), which are beneficial for health. 2. Cold Processed: The protein is cold-processed, meaning it’s not exposed to high heat during production. This helps maintain the integrity of the protein and keeps it undenatured, preserving its bioavailability and amino acid profile. 3. Undenatured Whey: Since the protein is undenatured, it retains more of the natural nutrients found in whey, such as immunoglobulins and lactoferrin, which can support the immune system. 4. Free From Additives: • GMO-Free: The product does not contain genetically modified organisms. • rBGH-Free: No recombinant bovine growth hormone is used in the dairy production, which is a synthetic hormone some farmers use to increase milk production. • Soy-Free & Gluten-Free: Suitable for people with soy or gluten intolerances or allergies. • No Added Sugar: Unflavored and unsweetened, allowing for flexibility in how you use it without added sweeteners.Nutritional Profile:While the exact nutritional profile might vary slightly depending on the batch, typically, a serving of this type of whey protein powder might contain: • Calories: Approximately 100-120 per serving • Protein: 20-25 grams per serving, making it a good source of complete protein • Fat: 0 grams • Carbohydrates: 0 grams, often minimal due to the lack of added sugars • Sodium: 50 mgBenefits: 1. Muscle Recovery & Growth: High in essential amino acids, especially BCAAs (Branched-Chain Amino Acids), which are crucial for muscle recovery and growth after exercise. 2. Supports Immune System: Contains immunoglobulins and lactoferrin that can enhance the immune system. 3. Versatile Usage: Because it’s unflavored and unsweetened, it can be added to a wide range of foods, from smoothies and shakes to baking recipes, without altering the taste.
READ MORESubscribe to get special offers, free giveaways, and once-in-a-lifetime deals.
